Before getting into the details about the test for antiphospholipid syndrome, it will be interesting to know a little about the condition itself and what happens to a person if he/she has this syndrome. Phospholipids are lipid particles that are the outermost layer of cells which play an important role in blood coagulation. So, what is antiphospholipid syndrome?
Antiphospholipid syndrome, also called as Hughes syndrome, is an autoimmune thrombophilia which means that the blood has an abnormal tendency to form clots within the circulation itself. It is characterized by
- Elevated levels of antiphospholipid antibodies (APA) in blood
- Arterial Thrombosis – Formation of blood clots within arteries, the clot is called a thrombus
- Venous Thromboembolism – Thromboembolism occurs when a part of thrombus detaches and obstructs the flow of blood in smaller blood vessels
- Loss of pregnancy or maternal/fetal death due to placental insufficiency, preterm labour, pre-eclampsia and intrauterine growth retardation (IUGR).
This clinical condition has a wide array of signs and symptoms depending upon the site, size and extent of a blood clot. Antiphospholipid syndrome can be primary or secondary, that is associated with other systemic illness.
Some Characteristic Features of Antiphospholipid Syndrome are:
- It is seen commonly in females during the 4th decade of life.
- Nearly 10-40% of patients of systemic lupus erythematosus (SLE) and up to 20% of patients with rheumatoid arthritis (RA) show elevated levels of antiphospholipid antibodies in the blood.
- Nearly 15-30% of patients with antiphospholipid syndrome have a valvular heart disease called Libman Sacks endocarditis or non-bacterial thrombotic endocarditis.
- Due to abnormal coagulability of blood, patients are at a significantly high risk of having the following:
- Neurological Manifestations – Cerebral venous thrombosis, convulsions, stroke transient ischemic attack (TIA), Guillain Barre Syndrome (GBS), psychotic disorders, transient global amnesia or myasthenia grevis.
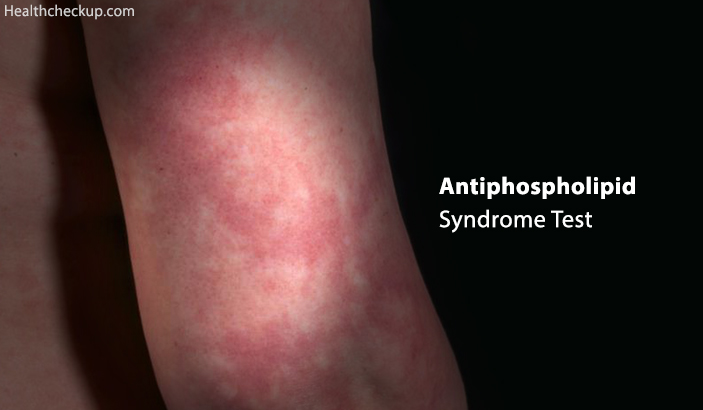
- Cardiovascular Manifestations – Myocardial infarction, stenosis, regurgitations of mitral and/or aortic valves, livedo reticularis (a purplish discolouration of skin due to swollen veins) and deep vein thrombosis.
- Obstetric Manifestations – Repeated or spontaneous miscarriage, fetal growth restriction and fetal death
- Renal Manifestations – Nephropathy, renal artery stenosis, renal vein thrombosis, acute or chronic renal failure or renal hypertension.
- Pulmonary Manifestations – Pulmonary hypertension, alveolar haemorrhage and adult respiratory distress syndrome (ARDS)
- Ophthalmological Manifestations – Infarction of the retinal artery and retinitis.
- Gastro-Intestinal Manifestations – Mesenteric and portal vein hypertension, intestinal, oesophagal or splenic perforation, ischemic colitis, ascites or pancreatitis.
- Endocrine Manifestations – Infarction and necrosis of suprarenal and pituitary glands have been documented.
- Haematological Manifestations – Hemolytic anaemia, hemolytic uremic syndrome, thrombotic thrombocytopenic purpura and disseminated intravascular coagulation.
- Catastrophic Antiphospholipid Syndrome – It is a severe form of an antiphospholipid syndrome characterized by the compromised function of at least 3 organs and multiple occlusions in big and small blood vessels (thrombotic storm). Organs commonly compromised are the kidneys followed by the liver and the heart, CNS and skin. The mortality rate is very high due to multiple organ failure.
Testing for antiphospholipid antibodies is advised when signs and symptoms are seen suggestive of blood clots such as shortness of breath, headaches or pain and swelling of extremities. Antiphospholipid syndrome is diagnosed on the basis of 3 blood tests
- Anti-cardiolipin antibody
- A beta-2 GP1 antibody test
- Lupus anticoagulant
Preparation
- This test does not require fasting or use of any special instruments as a part of preparation.
- You need to inform your doctor beforehand if you are on medications such as quinidine, phenytoin, procainamide and penicillin. These medications can cause an increase in blood levels of antiphospholipid antibodies.
Procedure
- A sample of blood is drawn from and to the laboratory for testing IgM and IgG antibodies.
- If the test results are positive, the patient is advised to undergo a repeat test after 12 weeks before making a definitive diagnosis.
- Tests need to be performed when the patient is clinically stable. The antiphospholipid antibody test is not to be done during an acute thromboembolic episode.
- The test should be done before beginning anticoagulant therapy.
- Patients with past or present history of syphilis may test false positive for antiphospholipid antibodies.
Results and Interpretation
Tests for antiphospholipid syndrome along with their normal reference range and interpretation
1. Anti Cardiolipin Antibodies
| Antibody type | Cardiolipin IgA | Cardiolipin IgG | Cardiolipin IgM |
| Negative | ≤11 | ≤14 | ≤12 |
| Indeterminate | 12 – 20 | 15 – 20 | 13 – 20 |
| Low to medium positive | 21 – 80 | 21 – 80 | 21 – 80 |
| High positive | > 80 | >80 | >80 |
The test results of anti-cardiolipin antibodies are given as a ratio between a patient’s serum and normal serum. The test is based on the principle of an enzyme-linked immunosorbent assay (ELISA). Elevated levels are diagnostic of antiphospholipid syndrome.
2. Lupus Anticoagulant: 20-39 GPL or MPL Units
Unlike other antibody tests, lupus anticoagulant is done in sequential tests.
- Activated partial thromboplastin time (aPTT) is also checked.
- Platelet counts may be reduced moderately if the patient is under anticoagulant therapy like heparin. In such cases, false positive results may be observed.
- Nearly 60% if patients with lupus anticoagulant also show elevated levels of anti-cardiolipin antibodies in the blood.
In Addition to Testing for Lupus, One or More of The Below Mentioned Tests may be Advised to Confirm the Presence of Lupus Anticoagulant:
- Platelet neutralization
- Hexagonal phase II phospholipid assay
- Kaolin clot time
- Prothrombin time
- Tissue thromboplastin inhibition test
- Coagulating factors
- VDRL
3. Beta-2 GP1 Antibodies: Less Than 15U/ml
- Elevated levels at two testing occasions indicate the presence of the antiphospholipid syndrome. ELISA principle is used to detect the presence of these antibodies.
- In general, anti-cardiolipin antibodies are commonly considered to be more a more reliable pointer for antiphospholipid syndrome.
- If tests for antiphospholipid antibodies show moderate to high values, it is considered positive if results are found to be persistently positive even after 12 weeks.
- Test results may vary depending upon age, gender, health status and history of previous infections or medications. Therefore test results are interpreted in correlation with clinical signs and symptoms of the patient.
Duration of the test
- The test begins withdrawing a sample of blood by performing a venepuncture. This does not require more than 5-10 minutes.
- You can expect the test results in 24-36 hours.
Dr. Himanshi is a Homoeopathic consultant and currently working as a lecturer in Post-graduate faculty of Homeopathy, Parul University, Vadodara. Completed BHMS and MD in Homeopathy in January 2018 and also has a clinical experience of about 6 years. Personal interests include reading, spending time with family and traveling.