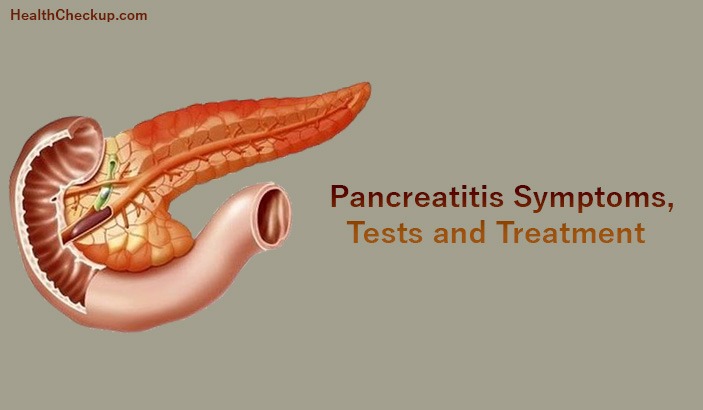
The term “Pancreatitis” refers to inflammation and swelling of the pancreas. The pancreas is a gland situated behind the stomach and next to the large intestine. The functions of the pancreas include releasing of digestive enzymes into the small intestine and releasing of hormones insulin and glucagon in to the blood stream. Pancreatitis or inflammation of the pancreas occurs when the powerful digestive enzymes are activated before they are released into the small intestine and they begin attacking the pancreas.
Types of Pancreatitis
There are two main types of Pancreatitis: Acute and Chronic
Acute Pancreatitis:
Acute pancreatitis involves sudden inflammation of the pancreas and it lasts for a short time. The symptoms of acute pancreatitis range from mild discomfort to bleeding in the gland, serious tissue damage, infection and cyst formation. The good thing is that acute pancreatitis is easily treatable and most people recover completely after receiving the right treatment. When it takes a severe from, it can harm other vital organs such as kidneys, lungs and heart.
Gallstones are the most prevalent cause of acute pancreatitis. Gall stones cause inflammation in both the pancreas and the bile duct. Alcoholism is also a potent cause of acute pancreatitis.
Chronic Pancreatitis:
Chronic pancreatitis involves long lasting inflammation of the pancreas and it causes permanent damage to the gland. Repeated inflammation of the pancreas leads to the formation of scar tissue which may affect the normal production of digestive hormones. As a result, the patient may have trouble in digesting fats.
Alcohol abuse is the leading cause of chronic pancreatitis. Autoimmune and genetic disease can also cause chronic pancreatitis.
Symptoms of Pancreatitis
One of the most common recognizable symptoms of acute and chronic pancreatitis is upper abdominal pain. Some of the other symptoms of pancreatitis include:
- Pain that radiates from your left side around to your back
- Indigestion
- Nausea and vomiting
- Abdominal tenderness
- Unexplained weight loss
- Bloating with a swollen stomach
- Fever
- Increased heart rate
- Hiccups
- Bleeding due to anemia
- Liver problems
- Nutritional deficiency due to mal-absorption
- Diabetes resulting from inability to produce insulin
Diagnosis of Pancreatitis
Diagnosis of pancreatitis involves a combination of blood tests and imaging scans. The blood tests reveal any rise in the level of pancreatic enzymes while the ultrasound, MRI and CT scan shows the size of the pancreas.
Pancreatic function test:
This test is done in order to find out whether the pancreas is producing the right amounts of digestive enzymes or not.
Blood Tests:
Blood tests help to evaluate the function of the gallbladder, liver and pancreas. Levels of pancreatic enzymes amylase and lipase are measured.
Secretin Stimulation Test:
This test measures the ability of the pancreas to respond to hormone secretin. Secretin in produced by the small intestine and it stimulates the pancreas to release a fluid that aids in digestion and neutralizes stomach acids.
Fecal Elastase Test:
This test also helps to determine the functions of the pancreas. It measures the level of enzyme elastase present in the patient’s stool. Elastase in an enzyme found in fluids produced by the pancreas. Its function is to break down proteins.
Glucose tolerance test:
This test is done to measure the damage to the insulin producing beta cells of the pancreas.
CT (Computed Tomography) Scan
This imaging test helps to access the health of the pancreas. It helps to indentify any complications or pancreatic diseases such as fluid around the pancreas, infection or collection of pancreatic enzymes, tissue or fluid.
Ultrasound:
Abdominal ultrasound helps to detect any gallstones that might block the flow of fluids from the pancreas. It also helps to indentify an abscess or pancreatic pseudocyst.
MRI (magnetic resonance imaging):
An MRI provides a clear picture of the bile ducts and pancreatic duct.
ERCP (Endoscopic Retrograde Cholangiopancreatography):
In this procedure, a tube is inserted down the throat, into the stomach and then small intestine in order to check the structure of the common bile duct and pancreatic duct on an X-ray.
Biopsy:
In this procedure, a small tissue sample from the pancreas is removed from the pancreas for the purpose of lab testing.
Treatment for Pancreatitis
Because the pancreas is an integral part of the digestive process so the treatment for both acute and chronic pancreatitis involves hospitalization for complete rest and recovery.
Treatment for Acute Pancreatitis
- Acute pancreatitis is treated with IV fluids and pain medications in the hospital.
- Patients suffering from severe form of acute pancreatitis need to be admitted to intensive care unit (ICU) where the patient is kept under constant watch because pancreatitis can damage the kidneys, heart and lungs.
- In case of death of pancreatic tissue, surgery may be required to remove the dead and damaged tissues.
- Acute pancreatitis caused by gallstones may require removal of the gallbladder or surgery of the bile duct.
Treatment for Chronic Pancreatitis
- In case of chronic pancreatitis, doctors will try to relieve the pain and improve the nutrition problems first.
- Patients are prescribed pancreatic enzymes and insulin.
- Surgery may be needed in some cases in order to relieve abdominal pain, restore proper drainage of pancreatic enzymes and hormones and treat chronic pancreatitis caused by blockage of the pancreatic duct.
Diet for Pancreatitis
Diet plays an important role in recovering from pancreatitis. People with acute pancreatitis are prescribed bowel rest for a few days. Bowel rest means no food or liquid intake by mouth. The patient is provided nutrition and fluids intravenously and the pancreas is given some time to recover. Then the patient is gradually advanced to oral intake of food starting with clear fluids, then soup and then solid foods.
Patients with chronic pancreatitis are suggested to have a low-fat healthy diet. The maximum fat intake is 20 g per day. The diet should be rich in carbohydrates though. Eating small sized and more frequent meals throughout the day put minimal stress on the pancreas. The patient should also drink lots fluids in stay hydrated.
Life-threatening complications such as pancreatic cancer, kidney damage and pancreatic infection can arise from chronic pancreatitis. Therefore, it is best to seek medical treatment right away in order to avoid these situations.
Medically Reviewed By