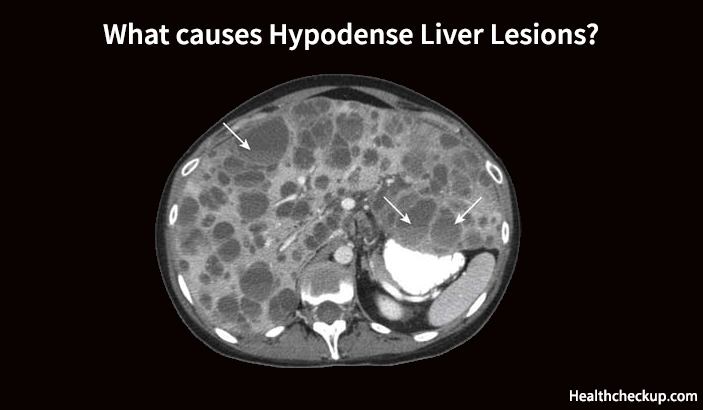
A Hypodense Liver Lesion or Hypodensity Liver is a deformity in the liver tissue that appears less dense than the surrounding tissue in radiological scans such as Computed Tomography (CT) scans or Magnetic Resonance Imaging (MRI). The appearance of these lesions in the radiological tests does not improve with the injection of intravenous contrast, and their presence may indicate a number of liver conditions including hemangioma, benign/malignant lesions, lipoma, liver abscesses, or simple hepatic cysts. Physicians use physical examination, the patient’s medical history, and clinical symptoms, and liver function tests along with CT scans or MRI to diagnose hypodense liver lesions.
What Causes a Hypodense Lesion on the Liver?
The causes of hypodensity liver lesions are many and they could include benign liver cysts that have no symptoms or malignant tumors which are usually associated with certain symptoms.
Sometimes a part of the liver tissue may become hypodense as compared to the nearby tissue due to focal fatty changes or due to primary or secondary tumors. If the entire liver tissue becomes hypodense, and especially if the mean attenuation is considerably less than that of the spleen, it suggests diffuse infiltration with fatty change. Also, a change in the liver density may appear radiologically if a contrast substance is administered during a CT scan.
The Detection of Liver Masses
Liver masses or lesions are usually detected on CT scans, and their visibility on these scans depends on the weakening difference between the lesion and the normal liver. Liver tumors are usually not detectable on a Non-Enhanced CT scan (NECT) because the characteristic contrast between the normal liver parenchyma and the tumor tissue is very low. The NECT is not very effective in detecting tumors comprising of fat, cystic components, calcifications, or haemorrhage, and therefore intravenous contrast must be used to enhance the visibility of these tumors in the scans.
Normally the liver has a dual blood supply. 80% of the blood supply to the liver parenchyma is by the portal vein and the rest of the blood supply, i.e. 20% is by the hepatic artery. When an IV contrast is administered to a patient, the enhance is seen in the portal venous phase, but the blood supply to any tumors in the liver is 100% through the hepatic artery, and therefore they will show enhancement in the arterial phase. Therefore, it should be understood that the different enhancement patterns between normal liver parenchyma and liver tumors are due to the difference in blood supply to the two types of tissue in the various phases of contrast enhancement.
The hypervascular tumors show enhancement in the arterial phase due to the enhancement in the hepatic artery, and the normal liver parenchyma does not show any enhancement in this phase because the contrast has not yet reached the portal venous system. These hypervascular tumors appear as hyperdense lesions in a comparatively hypodense liver tissue.
The same logic is used to detect hypovascular lesions in the liver. These lesions are detected in the portal venous phase when the normal liver parenchyma appears maximally enhanced. During this phase, the hypovascular tumors remain obscure and appear as hypodense lesions in a relatively hyperdense liver.
The contrast injection is in the equilibrium phase approximately 10 minutes after its injection, and the visibility of the tumors is maximal at this time because they either flush out the contrast at faster rate than the normal liver parenchyma or at a slower rate than the normal liver parenchyma. They either appear hypodense or hyperdense than the surrounding liver tissue.
Arterial Phase Imaging
A satisfactory arterial phase imaging depends on two important factors, i.e. optimal timing and the speed of contrast injection. Hypervascular tumors have been found to augment optimally after 35 seconds after the contrast injection is administered i.e in the late arterial phase. This is the time taken by the contrast to pass from the peripheral vein to the hepatic artery and to diffuse into a liver tumor if present.
The best arterial phase imaging results are obtained when the contrast is injected at the rate of 5ml/sec because this injection rate ensures better enhancement as more contrast is carried to the liver when the scanning is started and the contrast reaches the highest concentration during the arterial phase imaging when administered at this rate.
The Portal Venous Phase
The principle behind the portal venous phase imaging is precisely opposite to that of arterial phase imaging. The right time to start the scanning is in the late portal venous phase, i.e. approximately 75 seconds after the IV contrast has been administered. This is because the enhancement of the portal vein also starts at 35 sec, which is during the late arterial phase.
The late portal venous phase is also called the hepatic phase because the enhancement of the hepatic veins also takes place during this phase. If the hepatic veins’ enhancement is not seen at this phase, it means that the scanning is being done too early. In case only portal venous imaging is required, as in the case of the detection of hypovascular metastases in colorectal cancer, there is no need for fast contrast injection. An injection rate of 3ml/sec is sufficient because only the total amount of contrast is more important in this phase.
The Equilibrium Phase
The phase in which the contrast starts to exit the liver and the liver tissue starts to decrease in density is called the equilibrium phase. This phase begins after 3 to 4 minutes of administering the contrast and the best imaging results are obtained at about 10 minutes of contrast injection. Imaging is usually done in this phase to detect fast tumor washout in hypervascular tumors like those of Hepatocellular Carcinoma (HCC) or retention of contrast in the blood pool as seen in hemangiomas or the retention of contrast in fibrous tissue in capsules in case of HCC or scar tissue in focal nodular hyperplasia or Cholangiocarcinoma.
Relative Hyperdense Lesions in the Delayed Phase
Well-organized fibrous tissue that is dense takes a long time to let a contrast substance such as iodine or gadolinium in, and once the contrast is getting into the tissue, it takes a long time to get washed out in the equilibrium phase. The fibrous components of hepatic tumors usually appear brighter than the surrounding liver tissue when the contrast washes out. In the case of Cholangiocarcinoma, the delayed phase may be the only time that a tumor can be detected because the tumor tissue will appear lighter than the surrounding liver parenchyma as it is more washed out than the normal tissue.
Benign lesions follow a different type of contrast washout pattern. For example, in focal nodular hyperplasia or in case of an adenoma, the lesion will exhibit a fast enhancement in the arterial phase, and it becomes isodense in the portal venous phase and continues to stay isodense with the liver tissue even in the equilibrium phase. This pattern is displayed by the benign tumors due to the lack of sufficient neoplastic neovascularity to have a fast contrast wash out. Especially in cirrhotic patients, doctors rely on the delayed phase to differentiate a benign tumor that exhibits little enhancement from a hepatocellular carcinoma tumor.
What Do We Conclude..?
Considering all the aspects of hypodense liver lesions discussed above, it can be concluded that various benign conditions can be responsible for hypodense liver lesions or liver hypodensity, and not all causes imply malignancy. A comprehensive analysis of the patient’s medical history, his signs and symptoms, his family history, and possibly a biopsy will help the doctor make the right diagnosis and the causes for hypodense liver lesions.
Medically Reviewed By

I am an experienced Medical/Scientific writer with a passion for helping people live a happy healthy life. My thirst for writing has followed me throughout the years – it is there when I wake up, lingering at the edges of my consciousness during the day, and teases me at night as I go to sleep.