The arterial blood gas (ABG) test is used to measure the acidity (pH) and levels of oxygen (O2) and carbon dioxide (CO2) in the blood from an artery. It is essential for evaluating respiratory function and metabolism in patients, especially those with suspected respiratory distress or imbalance in blood pH.
Purpose of the Arterial Blood Gas Test
- Assessing Lung Function: The ABG test is crucial for evaluating a patient’s lung ability to oxygenate blood and remove carbon dioxide.
- Monitoring Treatment: It is used to monitor patients on mechanical ventilation and those receiving oxygen therapy for conditions like chronic obstructive pulmonary disease (COPD).
- Determining Acid-Base Status: Helps in diagnosing and monitoring disturbances in the body’s acid-base balance, which can be affected by conditions such as kidney disease, metabolic disorders, or drug overdose.
- Critical Care: Essential in emergency settings or intensive care units for immediate assessment of a patient’s respiratory and metabolic function.
Preparation for the Arterial Blood Gas Test
- Informed Consent: Patients should be informed about the purpose of the test and any associated risks.
- Positioning: The patient may need to rest in a certain position to access the artery easily.
- Medication and Health History: It is important to inform the healthcare provider about all medications being taken, as some can affect blood gas levels.
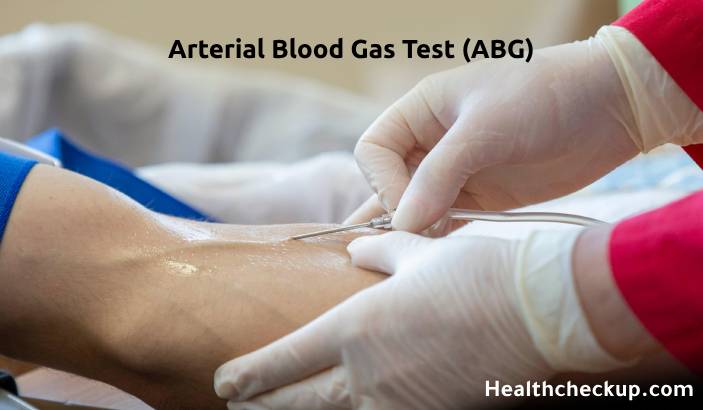
Procedure of the Arterial Blood Gas Test
- Site Selection: The test is typically performed on the radial artery in the wrist; other sites include the femoral artery in the groin or the brachial artery in the elbow.
- Blood Collection: A small amount of blood is drawn directly from the artery using a syringe. The area is first cleaned, and a local anesthetic may be applied to minimize pain.
- Immediate Handling: Arterial blood must be analyzed within a few minutes after collection to ensure accuracy, as blood gas levels can change rapidly once the blood is outside the body.
Normal Range
- pH: The normal arterial blood pH is between 7.35 and 7.45.
- Partial Pressure of Oxygen (PaO2): Normally ranges from 75 to 100 mmHg.
- Partial Pressure of Carbon Dioxide (PaCO2): Typically falls between 35 and 45 mmHg.
- Bicarbonate (HCO3): Normal plasma level is between 22 and 26 mEq/L.
- Oxygen Saturation (O2 Sat): Should be between 94% to 100%.
Results Interpretation
- Acidosis or Alkalosis: A pH below 7.35 suggests acidosis, while a pH above 7.45 indicates alkalosis.
- Respiratory or Metabolic Origin: Abnormal PaCO2 levels suggest respiratory issues, while deviations in HCO3 indicate metabolic causes.
- Hypoxemia: Low PaO2 may indicate issues with lung function or oxygen exchange, requiring urgent medical attention.
Risks Associated with the Arterial Blood Gas Test
- Discomfort or Pain: The most common complaint due to the nature of drawing blood from an artery.
- Bleeding and Bruising: Prolonged bleeding or hematoma at the puncture site, especially in patients with bleeding disorders or on anticoagulation therapy.
- Infection: Although rare, there is a risk of infection at the puncture site.
- Vascular Complications: Very rarely, damage to the artery can occur, potentially leading to vascular spasm or thrombosis.
The arterial blood gas test provides immediate and precise measurements of the gases and pH in arterial blood, offering essential insights into a patient’s respiratory efficiency and metabolic status. The ABG test can guide critical care decisions, particularly in emergency and intensive care settings, by helping to tailor treatments such as ventilation and medication administration.
I specialize in writing about health, medical conditions, and healthcare, drawing extensively from scientific research. Over the course of my career, I have published widely on topics related to health, medicine, and education. My work has appeared in leading blogs and editorial columns.